Part Three: A Historic Review of Extraction Orthodontic Treatment
- drwhitneyortho
- Oct 20, 2024
- 9 min read
Updated: Oct 21, 2024
“I see a whole lot of crowding, we’ve got to pull out four teeth.” For the third part of this series, we are pivoting to another controversial topic and longstanding debate: extraction versus non-extraction orthodontic treatment. We will review the origins of extraction treatment philosophies, a newer concept re-opening extraction spaces in adults, as well as assessing long-term outcomes.
Extraction orthodontic treatment was very common during my childhood and those of 1-2 previous generations; let’s say it peaked from the 1980s-2000s (am I aging myself?!). Truthfully, it still is popular today, however, it has also become a heated topic.
It’s time for another history lesson 😊 Please let me introduce Dr. Charles Tweed. Tweed popularized orthodontic extractions approximately eighty years ago(!). His rationale was based off of numerous facial profile skeletal (x-ray) analyses. Tweed defined what he considered the perfect angles of the teeth in relation to the maxillary or mandibular facial planes. The objective was to achieve facial harmony.
It was 1940 and there was a different set of esthetic and social principles, then. Tweed presented his findings when comparing facial esthetics in non-extraction to extraction treatments. Tweed believed that extractions (of premolars in particular) helped create a more harmonious profile and allowed for a decrease in dental relapse. Tweed had also shared that he was having trouble creating a balanced face with non-extraction treatments. He claimed that his patients with facial balance and harmonic proportions had lower incisors that were upright over the basal bone (Wahl, 2006). Meanwhile, he deemed those who had protruding incisors otherwise to have less visually favorable facial features.
In 1966, Tweed finally honed his cephalometric (skeletal) analysis, wherein he characterized the lower incisor position relative to the basal bone and face. This was coined as the diagnostic “facial triangle”, which was used as a guide in determining the ‘normal’ position of the teeth in relation to their respective jaw bones and head structure (Kumari and Das, 2017).
I wanted to share this excerpt from Dr. Tweed’s interview for the Journal of Clinical Orthodontics, which was published in 1968:
“the diagnostic facial triangle is a guide for the young man, a very accurate one in more than 95% of cases, but in the final analysis, the eye is the deciding factor.”
He also stressed the importance of correcting orofacial habits, which I think is often overlooked today by many clinicians:
“I refer each one of my patients that comes to me for an examination to the therapist for the correction of any abnormal tongue, lip, sucking, or swallowing habits--for to me, unless such habits are corrected, the face cannot develop normally and as beautifully as would be the case if the individual were free from the adverse effects of these influences.”
We will touch more on these important and often overlooked considerations in Part Four.
In summary, Tweed believed that the key to a successful correction of malocclusion was to position the mandibular incisors over basal bone (Merrifield, 1994). He was amongst several other pioneers who paved the path for these orthodontic analyses. Tweed calculated that the incisors needed to be perpendicular to the mandibular plane. The measurement is specifically called the IMPA (incisor-to-mandibular plane angle). As mentioned, according to Tweed, those with protruding incisors (let’s say >100 degrees) had less favorable facial features, esthetically speaking.
It’s important to clarify that Tweed, as well as many of the mid-20th century orthodontists used Caucasians to create their facial standards. Most orthodontists today would agree that one racial or ethnic group’s cephalometric “norms” likely does not correspond with that of other ethnic groups. Furthermore, the term “normal” was defined by Tweed (1966) as “the balance and harmony of proportions considered by the majority of us as most pleasing in the human face.”
The idea of “anchorage preparation” was another core Tweed principle. What this meant was that Tweed wanted to do everything possible to prevent mesial (i.e. forward) drift of teeth, especially in orthodontic extraction treatment. Teeth would be strategically pulled in segments. This would allow for maximum retraction of the teeth from the A-P (side) dimension (Tweed, 1953). Headgears were used a source of skeletal (versus dental) anchorage, especially in skeletally class II patients. Headgears apply a force in the A-P (side/profile) dimension. The headgear’s force (which could be quite heavy and dangerous!) would actually restrict anterior maxillary skeletal growth, allowing the mandible to play catch up. Essentially, those who use headgears were stunting skeletal growth to correspond (often times) to an under-developed mandible. We might imagine what the ramifications this might have on the airways in children and adults in later years…
As we discussed, Dr. Tweed very strongly supported extractions, and serial extractions were performed when there was severe crowding. Serial extractions are when baby teeth (such as the baby canines [C's] and/or primary molars [D's]) are pulled out first followed by the permanent premolars [4's]. What is the cutoff to determine this? Per his interview, >6 mm crowding seems to be his cutoff:
“If the tooth-basal bone discrepancy is 6mm or more, I certainly would begin a serial extraction procedure and eventually remove all four first premolars prior to any active treatment.”
Extractions are considered an orthodontic “camouflage” treatment. Camouflage means that the teeth are being moved/tipped to hide a skeletal discrepancy, as you can see in these jaw models below. Personally, I will rarely extract teeth unless I see >10 mm crowding, let’s say, or if a patient is a skeletal class III and refusing jaw surgery then I will try to achieve a positive overjet through dental camouflage treatment. We will visit this perspective in a bit.
Tweed’s diagnostic and treatment principles are still taught in academia. In present-day, there is a Tweed course that orthodontists, usually while in residency, may attend in Arizona for about ten days. There, one may perfect his/her wire bending skills and learn how to finish orthodontic cases to Tweed’s ideals.
Similarly, the Begg philosophy was first introduced in 1954 when Dr. Begg described the Stone Age Man’s attrition. From his studies of the aborigines, he concluded that the third molars migrated forward approximately half an inch between teen age and the time of its eruption. This migration was accomplished by the attrition (i.e. wearing down) of the contact areas and the occlusal surfaces. Begg also observed a very healthy condition of the gingiva in the aborigines. He suggested that one must resort to an artificial compensation of attrition by eliminating the four first premolars in conjunction with orthodontic treatment (Begg, 1965).
I feel like there were some missed connections, unfortunately. Perhaps tougher diets and an increased use of orofacial muscles would encourage skeletal growth. This in effect would also decrease crowding [this is the functional matrix theory, which I discussed here].
In this vein, many will recognize that the westernization of our diet and introduction of highly processed foods is one of the main causes of modern-day crowding and malocclusions. However, I suppose in the 1950’s and 60’s no one seemed to question these changes and their consequences. Instead, orthodontic innovators looked for “solutions” to compensate for them. Well, except for Dr. Haas in developing his palate expander (as discussed in Part Two), which interestingly did the opposite of what Dr. Tweed and Dr. Begg advocated.
As another aside, extraction treatment or non-extraction treatment for that matter may or may NOT actually affect facial profiles or soft tissue appearances. Extraction treatment may sometimes, particularly in those with thin soft tissues, make one’s nose or chin appear more prominent. One may also appear to have thinner lip tissues as he/she ages due to less skeletal support from the “extract and retract” treatment (we’ll talk about this more in a moment!) (Sarver, 2015). I think that this is one reason that extraction treatment has come into question. However, it is also not always the case. Some people will not have any visible soft tissue changes, with or without extractions. In fact, a study by Freitas and colleagues (2019) drew this very conclusion.
Therefore, in my clinical practice, l never promise soft tissue changes with treatment. Instead, I will recommend that a patient should see a plastic surgeon if they want to ensure a measurable change. I additionally wanted to clarify that some people might have extremely large teeth for an average-size mouth. This anatomically disproportionate relationship could be a rationale for dental extractions.

So let’s fast forward to 1989 and introduce Dr. Bill Hang, whose thoughts began to swing the pendulum. Dr. Hang coined the term “extract, retract, regret syndrome” or ERRS. Dr. Hang discusses the emotional and esthetic damage that is caused as a result of extraction treatment. He also suggests that extractions have airway and TMJ risk factors.
Dr. Hang has a website, https://ortho2health.com/ (and previously managed www.facefocused.com), which focuses on orthodontics and orthotropics. His treating principles are the direct opposite of Dr. Tweed and Dr. Begg’s philosophies. Dr. Hang discusses the damages of flattening of the face. Furthermore, he supports adult patients to reopen extraction spaces and regain the space that was lost. Dr. Hang suggests that it will take 6-12 months to reopen these spaces for future implant sites and an overall 12-18 month treatment time. I think that this is a very generous figure, as average orthodontic cases are 18 months long. Opening up spaces in adults is not quick and easy. They also might have periodontal concerns to keep in mind (as we discussed in Part One). Another limitation I think is that there is a lot of writing without research or references to back it up.
I try to stay level and not subscribe to any particular school of thought. Most important to me is the evidence. Some airway companies and appliances require practitioners to “buy in” to their system and pay 50k BEFORE they can prescribe their appliances to patients. And then there is pressure to get an ROI, which I know is controversial to say. To add, I think a lot of these companies have a cultish vibe (there I said it, and I might delete it later!).
The extraction and non-extraction debate has been ongoing, and is still discussed today. The American Association of Orthodontists (AAO) in 2019 published the White Paper on Obstructive Sleep Apnea (OSA) and its relationship to orthodontics. They briefly touched on the extraction/non-extraction question. I think it is important to remember that OSA is extremely complex and multifactorial, and I like to call it 4-dimensional. Teeth alone don’t necessarily influence airway dynamics or collapsibility. The AAO concluded that there was not a significant difference in OSA risk factors; however, their means of analysis was a bit on the surface. It is currently under re-review and likely to be modified. Coincidentally, also in 2019, the American Board of Orthodontics removed their requirement to present an extraction case to become a Board-Certified orthodontist. Perspectives and influences have definitely shifted.
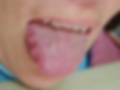
I generally favor an expansion treatment philosophy in terms of supporting overall (and thus also airway) growth and development. This I would hope will positively influence the soft tissue, although any definition of what this means is extremely subjective. The resting space for the tongue will also be more comfortable in a larger mouth. Fun fact: Whenever you see scallops on the sides of the tongue, which are indentations of teeth, that often suggests that there isn’t enough room for the tongue! I see these scallops all of the time (admittedly, even in my own mouth…ahh!).

I aim to extract as rarely as possible. However, sometimes there is no other option in order to establish a protected occlusion. More so if a patient refuses skeletal surgery or the other options discussed in Part Two. It’s important to review all treatment options, and the pros and cons of each of them. At the end of the day, I conjecture that the vast majority of orthodontists still extract teeth. I have never prescribed headgear or any appliance that restricts maxillary growth in my clinical practice. I typically reserve extractions for skeletal class III patients (i.e. those with underbites). These are cases where the lower jaw is too large relative to the upper jaw, and we will extract either an incisor or a set of premolars in the lower jaw. I may also discuss extractions when I see extremely severe crowding in adults. Generally speaking, I believe that patients today are more conservative, as well as more conscious in terms of the intersections of oral and medical health principles. Most patients I see want to save their natural teeth when possible.

Finally I want to remind that while we discussed heavily the extraction treatment tradeoffs, there are of course also risks and negatives for non-extraction treatment. In some cases, non-extraction and expansion cases might lead to teeth looking flared or proclined from the side/profile view. Some will feel that their soft tissue features are “too” full. There could also be a periodontal risks for recession or bone loss, especially if expansion is too aggressive. This can occur when teeth are pushed outside of the bony confines such as with the appliances discussed in Part One of this series. These risks need to be taken into consideration especially for adult orthodontic treatment, especially if there is no orthopedic or surgical component to treatment.
To conclude this series I will review and summarize early orthodontic treatment, airway and oromyofunctional therapy (OMT). Stay tuned!
Please contact author for references